Gut-Immune Connection: Exploring the Complicated Ties between Gut Health and Immunity
Introduction
Recently, researchers have discovered a fascinating connection that has profound implications for global health in their extensive investigation of the complex relationship between the gut and other parts of the body. The gut is sometimes referred to as “second brain” because it contains trillions of microorganisms which are called the gut microbiota, that play a major role in maintaining immune function and overall well-being. In this article we will venture into the developing science behind the gut-immune connection looking at how immune function is influenced by gut health.
A Microscopic Ecosystem: The Gut Microbiota
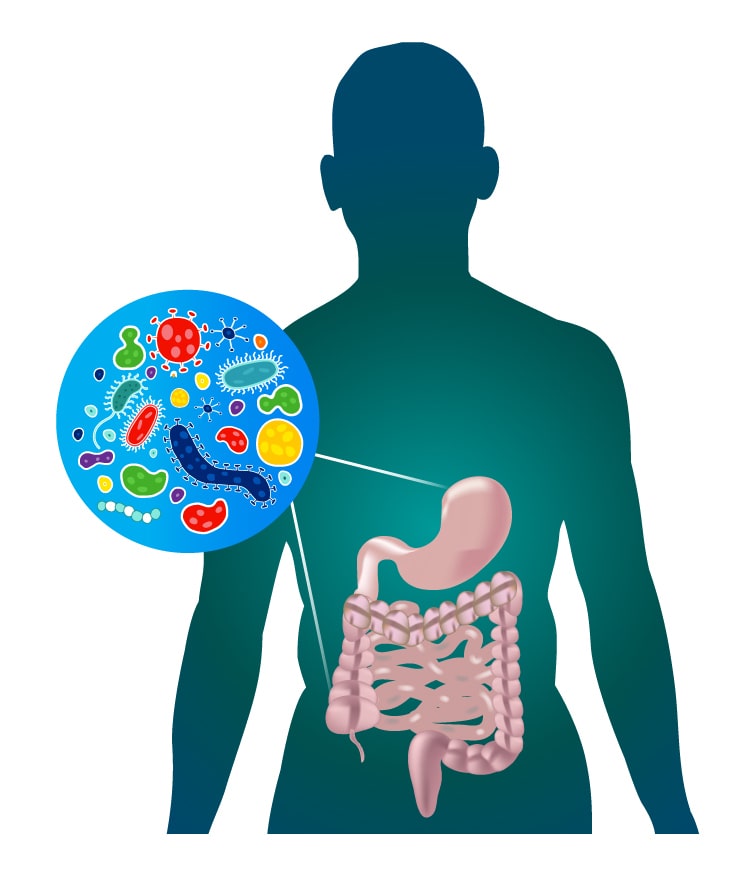
The human gut comprises a vast array of microorganisms such as bacteria, viruses, fungi, and archaea which make up what we know today as the gut microbiota. These microorganisms exist side by side delicately balanced each other’s presence creating a complicated system that contributes to digestion, nutrient uptake, metabolic activities and protection against diseases.
The diversity of these organisms is tremendous with over hundreds species living in gastrointestinal tract. A man’s or woman’s own bacterial makeup within one’s intestines results from various factors like genetics, diet habits, place of inhabitance and lifestyle choices just to mention but a few. Whilst some are beneficial to health others could be pathogenic on which they may contribute regarding health, other factors can cause disease, and when their balance is disrupted, disease occurs.
The Gut-immune Axis: A Two-way Highway
The gut-immune axis is a communication system that connects the gut to immunity and vice versa. The communication happens in different ways such as through signaling molecules, direct interactions between immune cells and the epithelial cells of the gut and modulation of immune response via products from microbiota situated in the gut.
One of its major roles is maintaining immune homeostasis which involves an equilibrium where the immune system can differentiate between harmful pathogens and helpful microorganisms as well as avoid non-specific immune responses towards harmless antigens like food particles or commensal bacteria.
Additionally, during early life development, the gut microbiota has an important role to play through educating and training the immune system so that it acquires appropriate responses as well as developing oral tolerance to dietary antigens and commensals. However, any disruption to this balance such as dysbiosis (an alteration in gut microbial composition) or damage to intestinal barrier could lead to impairment on all these functions resulting in compromised immunity; therefore making individuals prone to infections, autoimmune conditions, and inflammatory diseases.
Effects of Gut Health on Immune Function
Considerable proof implies that gut microbiota wellness directly influences immune function and inflammation throughout the body. An equitable and various gut microbiota is linked with improved immunity monitoring, greater anti-inflammatory cytokine production as well as enhanced barrier mechanism necessary for an effective immune reaction that guarantees resistance to illnesses.
Conversely, dysbiosis or changes in the gut microbiota structure have been connected to a variety of immune-based disorders such as inflammatory bowel disease (IBD), asthma, allergies, autoimmune diseases, and metabolic syndrome. The imbalance of gut microbial diversity that results in excess pathogenic bacteria or a decrease in commensal bacteria can result in chronic inflammation and abnormal immune responses thereby leading to tissue damage and progression of disease.
Besides, increasing evidence suggests that the metabolites generated by the intestinal microflora like short-chain fatty acids (SCFAs), bile acids and microbial antigens may be involved in modulating systemic immunity as well as inflammatory response. These compounds can influence immune cell activity, inflammation and metabolism through interaction with immunoglobulin cells located within the intestines or other tissues.
Microbiome Nutrition and Gut Health: Feeding the Microbes
Diet is among the most important variables affecting gut health and microbiota composition. The foods we consume are what the gut microbiota rely on for nutrients and energy, determining the make-up and functioning of this system. On the one hand, a diet full of fiber, prebiotics and plant-based products help to grow beneficial bacteria while enhancing the functioning of gut barriers; however, a high intake of processed foods, sugars or saturated fats can lead to an imbalance in gut microflora as well as proinflammatory response.
Such fiber-rich produce as fruits, vegetables, whole grains, legumes and nuts are very useful for maintaining our gut health because they serve as foodstuffs for some helpful bacteria that live there encouraging their development and diversity. Also probiotic fermented foods like yogurt, kefir, sauerkraut or kimchi have been used to restore healthy microbial balance in the gastrointestinal tract.
Also certain dietary components including polyphenols from fruits, vegetables as well as tea together with omega-3 fatty acid in fatty fish such as flaxseeds or walnuts have shown anti-inflammatory properties immunomodulatory activities so supporting intestinal wellness immunity respectively.
Lifestyle Factors and Gut Health
Apart from diet, different lifestyle factors can affect the gut health and immune system functioning. Activities such as exercises, handling stress levels, quality sleep and environmental exposures contribute to development of microbiota in gut and modulation of immunity.
Research has shown that regular physical activity increases diversity of gut microbiota, reduces inflammation and enhances immune function. It is known that moderate-intensity exercise like brisk walking, cycling or swimming lead to production of anti-inflammatory cytokines for growth of beneficial bacteria in the intestines.
However, stress may have negative effects on the immunity and also be harmful to the health of your digestive system. In effect, it has been witnessed that chronic stress leads to an altered composition of the microbial environment within the gut resulting in leaky bowel syndrome as well as compromised immunity consequently leading to systemic inflammation that would make you more vulnerable to attacks by infections as well as develop into chronic diseases.
Conclusion: Fostering the Gut-Immune Connection
In conclusion, the gut-immune connection is a captivating frontier in our understanding of human health and disease. This shows how vital it is to maintain a healthy gut system for overall good health and resistance against diseases because there is an intricate interplay between gut microbiota and the immune system.
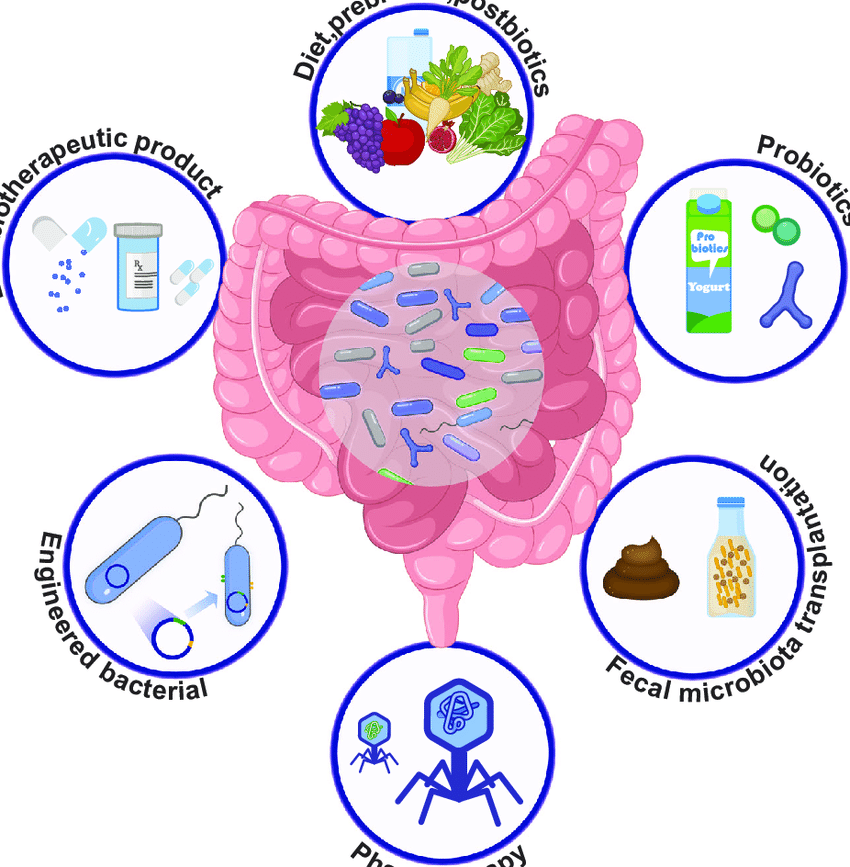
When we focus on our gut health through balanced diet, lifestyle changes, and intentional interventions, we will be able to support the immune response, minimize inflammation and sustain optimal health from inside out. By ensuring that our foods are filled with fibrous contents as well as fermented ones containing probiotic components; managing stress properly and taking part in physical activities, we can transform simple acts into enormous impact towards sound gastrointestinal health as well as strong immune systems.
With each day that passes by, research continues disentangling confusion around this complex relationship between the gut and immunity such that novel insights will emerge leading to new therapeutic strategies to prevent, treat diseases or palliate them. In short by developing mutually advantageous connection between our bowel systems and our immunity then we lay down basis of solid foundation for healthy existence in changing world.